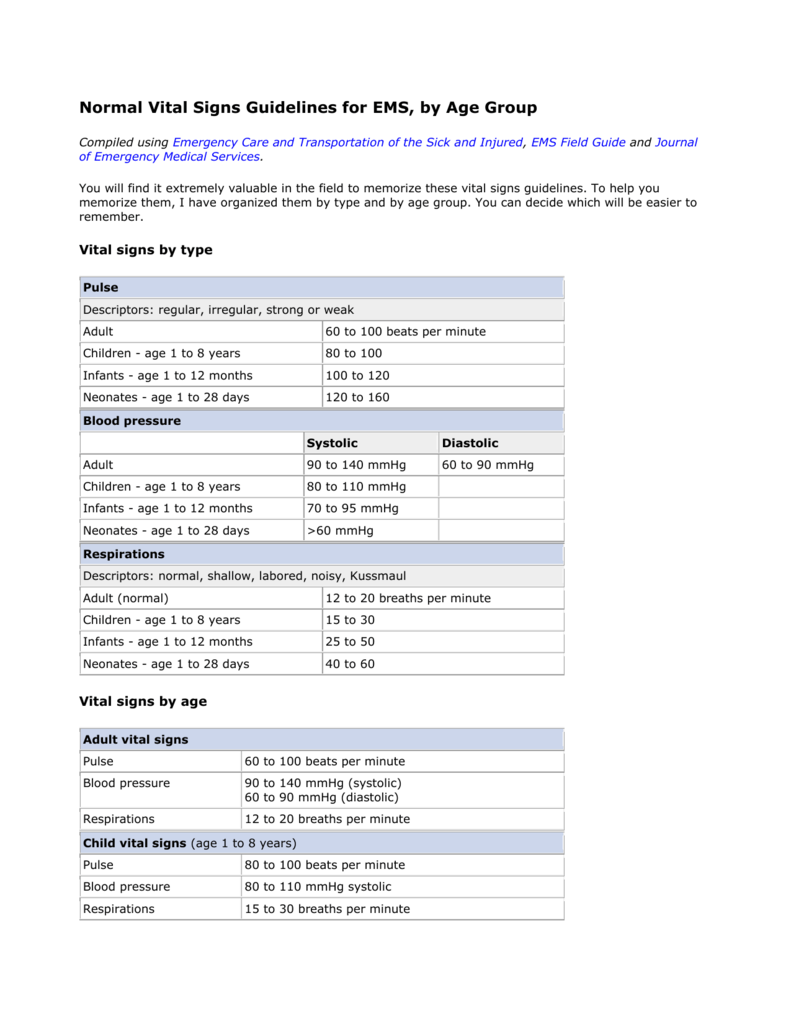
- You will need to know some things about tempo to play the piano or keyboard. Like heartbeats, musical beats are measured in beats per minute. A certain number of beats occur in music every minute. When a doctor tells you how fast your heart is beating, you can think, “Who cares?” But when a composer.
- Normal sinus rhythm is generally defined as between 60 beats and 99 beats per minute. Sinus Bradycardia There are a number of circumstances in which it's normal for the sinus rhythm to be at the low end of the range of beats per minute or at the high end.
- Normal Beats Per Minute Heart Rate
- Target Heart Rate
- Normal Beats Per Minute Woman
- Normal Adult Pulse Rate Chart
- Normal Beats Per Minute Dog
What is arrhythmia?
Normal Beats Per Minute Heart Rate
A normal pulse rate for a healthy adult at rest ranges from 60 to 80 beats per minute. Women tend to have faster pulse rates than men. A normal resting heart rate for adults between 18 and olderes counts between 60 and 100 beats per mnt, the normal resting heart rate is between 70 and minute (bpm).Hence, you run under the normal range of heart beats per minute.
Usually, a heart beats between 60 and 80 times per minute, but everyone has their own normal heartbeat rhythm. Some hearts beat faster or more slowly than others. When you are diagnosed with arrhythmia, it is an abnormal heart rhythm for you, but not necessarily for someone else.
The pumping action of your heart is triggered by electrical impulses that begin in your heart's natural pacemaker, called the sinus node (also called sinoatrial or SA node). Learn how a healthy heart works.
Arrhythmia may cause your heart to beat too slowly (bradycardia, less than 60 beats per minute) or too quickly (tachycardia, more than 100 beats per minute), or cause uncoordinated contractions (fibrillation).
Types of arrhythmia
Arrhythmias are defined by the speed of the heartbeats: slow and fast. They include bradycardia and tachycardia, with a variety of conditions under those two categories.
1. Slow heartbeat - bradycardia
Bradycardia occurs when your heart beats so slowly that it cannot pump enough blood for your body's needs. Untreated bradycardia can cause excessive tiredness, dizziness, light-headedness or fainting. An electronic pacemaker can help the heart to beat normally.
Bradycardia can be caused by:
- Sick sinus syndrome
This is a malfunction in the heart's natural pacemaker (the sinus node), which makes it fire too slowly. This condition may be caused by growing older or by disease. Some medications can also cause or aggravate a slow heartbeat. The resulting arrhythmia may be temporary or permanent. It can be treated with medication or with an electronic pacemaker. - Heart block
This is the slowing down or interruption of the electrical signal to the lower chambers of the heart which cause the heart muscle to contract. The heart's electrical system normally sends signals from the upper chambers of the heart (atria) to the lower chambers (ventricles) in a pattern that causes a heartbeat, a coordinated contraction of the heart muscle.

2. Rapid heartbeat - tachycardia
Tachycardia occurs when your heart beats too fast. There are two main types: Tachycardia above a ventricle and Tachycardia in a ventricle. Run.
- Tachycardia above a ventricle (supraventricular)
These are rapid heartbeats in the atria (the top chambers of your heart) or in the AV (atrioventricular) node – the electrical connection between the atria and the ventricles (the lower chambers of your heart). - Atrial flutter
In atrial flutter, an extra or early electrical impulse travels around and around the atria in a circular path rather than down along its normal path. This electrical signal causes the atria to 'flutter,' contracting at a much higher rate than normal. Atrial flutter is usually not life threatening, but can cause chest pain, faintness or other more serious problems. - Atrial fibrillation(Afib)
This common form of tachycardia occurs when the electrical activity in the atria is disorganized and very rapid. The pattern of electrical activity stimulates the atria randomly and at a high speed, which causes a series of very rapid contractions of the heart's upper chambers, preventing them from pumping effectively. Though not usually life-threatening, the rapid, irregular and uncoordinated beating of the ventricles may cause light-headedness or palpitations. If it goes on for several days or longer, it may increase your risk of stroke, because blood trapped in the atria can clot and travel from your heart to your brain, causing a stroke. - Paroxysmal supraventricular tachycardia (PSVT)
This type of tachycardia produces heart rates between 140 and 250 beats per minute. PSVT usually occurs in people who are born with an extra electrical circuit or pathway between the atria and the ventricles. PSVT often starts when you are young, but it may also start later in life. It may be distressing, but it is rarely life-threatening. - Wolff-Parkinson-White (WPW) Syndrome
If you have WPW syndrome, an extra, abnormal electrical pathway in your heart leads to tachycardia. The abnormality is present at birth (congenital), but WPW is usually diagnosed in adolescence or early adulthood. Most people with WPW syndrome lead normal lives. Many have no symptoms and have no episodes of tachycardia. Some people experience rapid heartbeats (paroxysmal supraventricular tachycardia), with heart rates rising up to 240 beats per minute. Other symptoms include palpitations, shortness of breath, fainting and possibly angina.
Tachycardia in a ventricle
- Ventricular tachycardia
Ventricular tachycardia occurs when the ventricles (the lower chambers of the heart) beat too fast. The ventricles are responsible for pumping blood to the rest of the body. If tachycardia becomes so severe that the ventricles can't pump effectively, it may be life threatening. Ventricular tachycardia can be treated with medications. Other treatments include an implantable defibrillator, catheter ablation, non-surgical procedures to destroy malfunctioning cells, or surgery to remove damaged heart tissue.
- Ventricular fibrillation
Incorrectly timed electrical signals or signals that do not follow normal pathways, may set off ventricular fibrillation. Like atrial fibrillation, the electrical signal that normally triggers a heartbeat splits and goes off on random paths around the ventricles instead of following its normal route. This causes a series of rapid – but ineffective – contractions of the ventricles. Without treatment, ventricular fibrillation may be fatal. Treatment is an electric shock to the heart, using a machine called a defibrillator. The shock resets the heart and returns it to its normal rhythm.
- Postural orthostatic tachycardia syndrome (POTS)
POTS makes it difficult to adjust to a standing position from a lying down position. People with POTS experience a rapid heartbeat that can increase up to 120 beats per minute within 10 minutes of standing. Other common symptoms include headaches, light-headedness, inability to exercise, extreme fatigue, sweating, nausea, chest discomfort, brain fog (mental clouding) and near fainting (syncope).
POTS commonly appears between the ages of 12 and 50 and typically affects more females than males. To diagnose POTS, your doctor will measure your blood pressure and heart rate while you’re lying down and standing up. Measurements are taken immediately after changing positions, as well as at 2, 5 and 10 minute intervals after standing up. POTS is frequently misdiagnosed as panic attacks or chronic anxiety. Sometimes a test called a head upright tilt table exam will be performed to help confirm the diagnosis.
Download we chat for mac. Although POTS can be a severely debilitating disorder, many patients will slowly improve over time and the majority will respond to treatment.
Causes
Electrical system malfunctions that lead to a heart rhythm disorder can be caused by many things. The list includes:
- damage to the heart from a heart attack
- thyroid problems
- caffeine
- drugs and supplements
- sleep apnea
Symptoms
There are many types of arrhythmias, some have no symptoms or warning signs, some are not very serious and others may be life-threatening.
Symptoms vary from person to person depending on how healthy your heart is and the type of arrhythmia you have, how severe it is, how often it happens and how long it lasts. Some arrhythmias do not have any warning signs.
Arrhythmias may decrease the blood flow in your brain and body causing heart palpitation, dizziness, fainting or even death. If you have bradycardia, you may feel tired, short of breath, dizzy or faint. If you have tachycardia, your heartbeat might feel like a strong pulse in your neck or a fluttering, racing beat in your chest. You may also feel discomfort in your chest, weakness, shortness of breath, faint, sweaty or dizzy. If you have any of these symptoms, see your doctor immediately.
Diagnosis
Your healthcare provider will review your medical history and give you a complete physical exam. They may also run tests:
Treatment

Arrhythmias may be treated with lifestyle changes, medications, surgery or other non-surgical techniques. Treatment depends upon the type of arrhythmia and how often you have episodes of arrhythmia.
Medications
Your doctor may prescribe medications to stabilize your heart rhythm:
Blood thinners may be prescribed to prevent blood clots.

Surgery and other procedures
Sometimes medications and lifestyle changes may not work for you and surgery is needed. These techniques could include:
Lifestyle
Most people with an arrhythmia can lead normal, active lives. Sometimes, lifestyle changes such as avoiding stress, and cutting out alcohol and caffeine (coffee, tea, soft drinks, chocolate, and some over-the-counter pain medicines) may be helpful. There are many other important lifestyle changes you can make that can improve your condition including eating a healthy diet and becoming more physically active. Talk to your doctor about the most beneficial lifestyle changes for you.
Living with arrhythmia
It’s normal to feel worried or afraid after a diagnosis of heart disease. Find someone you can turn to for emotional support like a family member, friend, doctor, mental health worker or support group. Talking about your challenges and feelings could be an important part of your journey to recovery.
- The recovery and support section is full of practical advice and tips to support you on your recovery journey.
- Find peer support resources here.
- Download or order our free book Living Well with Heart Disease.
- Join Heart & Stroke’s Community of Survivors or Care Supporters’ Community support groups.
- Sign up for the Heart & Stroke recovery newsletter. Get the latest research news and information, with tips and strategies to help you manage your recovery.
Related Information
To find useful services to help you on your journey with heart disease, see our services and resources listing.
How a healthy heart works
Living Well with Heart Disease
Recommended for you
Groups help you stay up to date with the information and resources that matter to you.
Looking for support?
Check out our support & recovery section
Multifocal atrial tachycardia (MAT) is a rapid heart rate. It occurs when too many signals (electrical impulses) are sent from the upper heart (atria) to the lower heart (ventricles).
The human heart gives off electrical impulses, or signals, which tell it to beat. Web design trends you can try right now. Normally, these signals begin in an area of the upper right chamber called the sinoatrial node (sinus node or SA node). This node is considered the heart's 'natural pacemaker.' It helps control the heartbeat. When the heart detects a signal, it contracts (or beats).
The normal heart rate in adults is about 60 to 100 beats per minute. The normal heart rate is faster in children.
In MAT, many locations in the atria fire signals at the same time. Too many signals lead to a rapid heart rate. It most often ranges between 100 to 130 beats per minute or more in adults. The rapid heart rate causes the heart to work too hard and not move blood efficiently. If the heartbeat is very fast, there is less time for the heart chamber to fill with blood between beats. Therefore, not enough blood is pumped to the brain and the rest of the body with each contraction.
Target Heart Rate
MAT is most common in people age 50 and over. It is often seen in people with conditions that lower the amount of oxygen in the blood. These conditions include:
- Chronic obstructive pulmonary disease (COPD)
- Lung failure
You may be at higher risk for MAT if you have:
- Had surgery within the last 6 weeks
- Overdosed on the drug theophylline
- Sepsis
When the heart rate is less than 100 beats per minute, the arrhythmia is called 'wandering atrial pacemaker.'
Some people may have no symptoms. When symptoms occur, they can include:
- Chest tightness
- Sensation of feeling the heart is beating irregularly or too fast (palpitations)
- Weight loss and failure to thrive in infants
Other symptoms that can occur with this disease:
A physical exam shows a fast irregular heartbeat of over 100 beats per minute. Blood pressure is normal or low. There may be signs of poor circulation.
Tests to diagnose MAT include:
Normal Beats Per Minute Woman
- Electrophysiologic study (EPS)
Heart monitors are used to record the rapid heartbeat. These include:
- 24-hour Holter monitor
- Portable, long-term loop recorders that allow you to start recording if symptoms occur
If you are in the hospital, your heart rhythm will be monitored 24 hours a day, at least at first.
If you have a condition that can lead to MAT, that condition should be treated first.
Treatment for MAT includes:
- Improving blood oxygen levels
- Giving magnesium or potassium through a vein
- Stopping medicines, such as theophylline, which can increase heart rate
- Taking medicines to slow the heart rate (if the heart rate is too fast), such as calcium channel blockers (verapamil, diltiazem) or beta-blockers
MAT can be controlled if the condition that causes the rapid heartbeat is treated and controlled.
Complications may include:
- Reduced pumping action of the heart
Call your health care provider if:
- You have a rapid or irregular heartbeat with other MAT symptoms
- You have MAT and your symptoms get worse, do not improve with treatment, or you develop new symptoms
To reduce the risk of developing MAT, treat the disorders that cause it right away.
Olgin JE, Zipes DP. Supraventricular arrhythmias. In: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier; 2019:chap 37.
Normal Adult Pulse Rate Chart
Zimetbaum P. Supraventricular cardiac arrhythmias. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 58.
Normal Beats Per Minute Dog
Updated by: Micaela Iantorno, MD, MSc, FAHA, RPVI, Interventional Cardiologist at Mary Washington Hospital Center, Fredericksburg, VA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
